For many years Pelvic disorders weren’t discussed much in our society and many women, and also men, have suffered in silence. In the last decade, Pelvic Health has become a point of interest for many people and therapists as well. The scientific studies related to Pelvic disorders and Pelvic treatment are increasing every day and finally, we are proud to confirm that specifically trained healthcare professionals can support and improve your Pelvic Health.
For best understanding, it is essential to learn about the Pelvic floor:
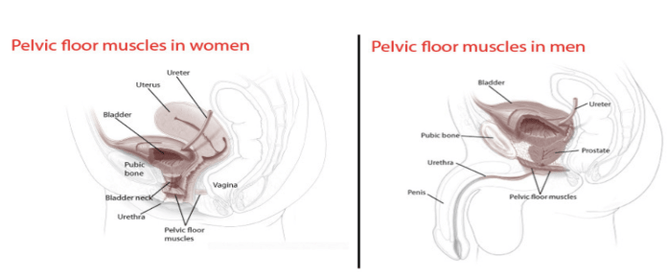
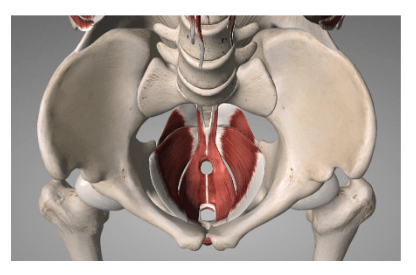
Pelvic floor anatomy:
The pelvic floor is the complex formed by fascial tissues such as ligaments and
pelvic muscles. In particular, we can recognise iliococcygeus, puborectalis,
pubococcygeus, coccygeus, ischiocavernosus, superficial and deep transverse
perineal muscles. These soft tissues find attachment to the bones at the bottom of
the pelvis. The pelvic organs include the urethra, bladder, intestines and rectum. If
you are a female, the pelvic floor and fascial tissues, also connect the uterus, cervix,
and vagina.Pelvic floor role:
The pelvic floor plays an important role in our body.
It supports and prevents the prolapse of the pelvic organs, including the bladder, urethra, rectum, anus, prostate, uterus, cervix, vagina and intestines;
It maintains the functionality of the urinary and rectal sphincters for continence;
It manages abdominal and pelvic pressures;
During pregnancy, the pelvic floor offers support to the baby and also assists in childbirth.
It’s vital for sexual health function. In females, the pelvic floor contributes to sexual sensation and orgasm; in males, it helps maintain an erection;
It stabilises hips and spine, especially when walking, standing and during physical exercises.Pelvic floor disorders:
When pelvic floor muscles are weak or malfunctioning, they lose the ability to fully play their role in supporting the pelvic organs, causing pelvic floor disorders.
These disorders can include urgency or stress urinary incontinence, overactive bladder, faecal incontinence and pelvic organ prolapse. They might cause symptoms like pelvic pressure or fullness, frequent urge to urinate or painful urination, lower back pain, difficulties with bowel movements, pain with sexual intercourse, pain in the pelvic region or genitals and pelvic muscle spasms.
Pelvic floor dysfunction can also occur with pregnancy, after childbirth, as a result of vaginal delivery with levator ani muscle avulsion or scarring from vaginal and/or perineal tear, age, menopause, surgery, repeated heavy lifting, prolonged sitting, tailbone or other pelvic trauma, sexual abuse, or conditions that create pressure on the abdomen, such as excessive weight, frequent coughing, laughing or sneezing.
Additionally, certain habits, symptoms, or conditions can contribute to pelvic floor disorders, such as endometriosis, dysmenorrhea (painful period or menstrual cramps), irritable bowel syndrome, interstitial cystitis, and habitual patterns of avoiding or restricting bowel movements.
Fortunately, there are nonsurgical ways to treat pelvic floor disorders and a good option to improve the functionality of this fascia tissue is to re-educate the pelvic floor with specific exercises.
Pelvic Health Internal Examination:
We are proud to let you know that at City Osteopaths you can now see Dr Giulia Buczkowsky for your pelvic examination.
Osteopath Giulia has completed post graduate training in Pelvic Floor Health, to educate you about your pelvis, explain what is happening, give appropriate exercises and perform the pelvic internal examination and treatment.
What does the internal examination consist of?
Depending on your pelvic issues, the internal examination includes vaginal and/or rectal assessment.
How is the internal examination performed?
The skilled therapist will put on sanitised gloves and examine the outside and inside of your vagina and/ or anus looking for:
Visible anatomical abnormalities
Avulsion, scarring and tearing
Pelvic organ prolapses
Muscle activity of the pelvic floor
What is the preparation for the internal examination?
Our first goal for internal examination is YOUR safety and comfort. Usually, Giulia prefers to have a chat during the osteopathic treatment before the internal health treatment, in order to answer all possible questions and concerns that might come up in an assessment. We feel it’s very important to provide all the information before the internal examination so you know what is going on with your health. As soon as the verbal consent is obtained, the internal treatment may be performed.
What is done during the internal examination?
Once the diagnosis is made, the therapist will provide a specific treatment program composed of pelvic floor exercises and pelvic re-education treatment with lifestyle habits change, toileting and sexual assistance.
Internal and Osteopathy:
Studies have shown the efficacy of the osteopathic manual treatment for pelvic floor dysfunction.
In addition to the pelvic health internal treatment, the osteopath will also conduct osteopathic manual therapy.
References:
Bi, X., Zhao, J., Zhao, L., Liu, Z., Zhang, J., Sun, D. and Xia, Y. (2013) ‘Pelvic floor muscle exercise for chronic low back pain’, Journal of International Medical Research, 41(1), pp. 146-152.
Eickmeyer, S. M. (2017) ‘Anatomy and Physiology of the Pelvic Floor’, Physical Medicine and Rehabilitation Clinics of North America, 28(3), pp. 455-460.
Kahyaoglu Sut, H., & Balkanli Kaplan, P. (2015) ‘Effect of pelvic floor muscle exercise on pelvic floor muscle activity and voiding functions during pregnancy and the postpartum period’, Neurourology and Urodynamics, 35(3), pp. 417-422.
Radzimińska, A., Strączyńska, A., Weber-Rajek, M., Styczyńska, H., Strojek, K. and Piekorz, Z. (2018) ‘The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: a systematic literature review’, Clinical Interventions in Aging, 13, pp. 957-965.